Local preventive interventions for smoking cessation improvement needed
Abbondanzieri A,1 Lucaroni F,2 Ingravalle F,1 Cecchetti L,1 Nucerito C,4 Ruscio V,3 Coia M,3 Ruscitti L E,3 Perra A3
1 School of Hygiene and Preventive Medicine, University of Rome Tor Vergata, Rome, Italy
2 Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome, Italy
3 Department of Prevention and Public Health, ASL Roma 5, Rome, Italy
4 Department of Mental Health and Pathological Addictions, ASL Roma 5, Rome, Italy
Introduction
Tobacco smoking represents a leading cause of preventable disease worldwide.1 It is responsible for the significant increase - by 3 to 5 times - in the incidence of both neoplastic and non-neoplastic disorders, such as chronic obstructive pulmonary disease, emphysema and coronary artery disorders.
Globally, over 1.1 billion people aged over 15 smoked tobacco in 2016, with a decreasing trend of smoking prevalence rate during the past 30 years.
In Italy one in four (26%) adults aged 18-69 is a current smoker. The average daily consumption is nearly 12 cigarettes per capita, although a quarter of smokers consumes more than one packet a day.3
Cigarette smoke kills more than 8 million people per year worldwide, nearly 80,000 in Italy.2 It is broadly ascertained that the regular use of tobacco products, because of its high concentration in nicotine, often leads to addiction, a phenomenon with important physiological, psychological and socio-economic implications.4-9 Nicotine exerts its action by binding to a subtype of cholinergic receptors, the nicotinic receptors, expressed in several regions of the central and peripheral nervous system,6,10,11 favoring the release of a number of neurotransmitters, including glutamate, GABA, dopamine, and norepinephrine.12-15 When nicotine concentrations decrease, excess receptors expressed at the membrane level exit the desensitized state, resulting in hyperexcitability of the cholinergic processes. This could explain the nervousness and tension that drive the smoker to consume the next cigarette and why smokers often report that smoking during the day helps them concentrate and stay relaxed.16,17 It has been broadly demonstrated that, avoiding nicotine for a few weeks, the number of nicotinic receptors returns to normal levels.18,19,20 Based on these observations, therefore, quitting smoking should not be difficult. However, most attempts to quit smoking fail.6,8,21,22 Evidence of interventional studies aimed to promote smoking cessation - mobile phone-based interventions,23 enhancement of partner support,24 internet-based intervention,25 physician advices26 and Quit and Win contest27 - is available at the moment, but with inconsistent results.
According to the guidelines promoted by the Italian Society of Tobaccology (Sitab) and the European Network for Smoking and Tobacco Prevention (ENSP), the smoking addiction treatment should be focused on different approaches: pharmacological (such as varenicline, bupropion, cystine, nicotine replacement therapy), psychological (such as cognitive-behavioral therapy, individual counselling) or combined approach.28 In Italy, the promotion of smoking cessation is mainly entrusted to the anti-smoking centers at the Local Health Units.
Aim of this study is to evaluate which factors influence the effectiveness of a primary preventive intervention focused on smoking cessation, set up by a Local Health Unit in Rome, Italy.
Materials and Methods
Population
Between February 2014 and December 2018, a pool of cigarette smokers was recruited by a center for smoking cessation called “CeSTab” (Centro per lo studio ed il trattamento del tabagismo), through public advertising, educational and social events. A retrospective observational cohort study was than performed on the data collected in the medical records of these users.
After a first individual meeting, aimed to record personal data of the enrolled subjects, those who voluntarily had decided to undertake treatment protocol were included in the study.
Subjects who had not finished yet the treatment program in December 2018 (n= 11) were excluded. It has not been possible to reach 20 more users, mainly because of the telephone number no longer reachable during the data collection phase.
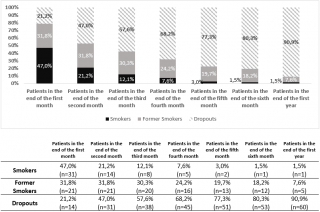
Smokers and non-smokers were defined according to the operational definitions of the World Health Organization (Table 1).31
Table 1. WHO Operational definitions of smoker.
Dropouts were those subjects who have decided to abandon the program at an early stage, despite three contacts attempts.
In order to identify associated factors with treatment effectiveness, univariate and multivariate binary logistic regression models were utilized.
Intervention
According to the latest guidelines,28 the treatment protocol included a first visit and subsequent follow-ups, generally monthly, up to one year, or according to the patient needs.
The first individual meeting consisted in a multidisciplinary evaluation, including medical, psychological and toxicological examinations.
The medical examination comprised anamnesis, instrumental exams and the measurement of expired CO and carboxyhemoglobin (COHb). Psychological examination was focused on the evaluation of the motivational state, the severity of addiction and the staging, according to Prochaska’s and Di Clemente’s “Trans-Theoretical Model of Change”.29 Finally, toxicological examination included the assessment of personal behaviors and habits, by administering specific tools, such as Fagerström test for nicotine dependence,30 visual addiction scale, self-efficacy test and motivational test.
Patients who decided to begin the program were generally treated with a combined (pharmacological and psychological) therapy, depending both on counselors’ advice and subjects’ compliance.
At each follow up, medical visit, toxicological examination and psychological support were performed.
Any eventual missing information were recovered by patient interviews.
Outcomes
Cigarette smoking cessation at 12th month from the beginning of the treatment program was evaluated as primary outcome. At the same time, changes in expired CO and COHb were evaluated as additional proxy of the effectiveness of the therapeutic program.
Moreover, to evaluate the effectiveness of the intervention, success rate, retention rate and attrition rate were estimated and illustrated through a cascade analysis.
Success rate was defined as the number of subjects who quit smoking 1, 2, 3, 4, 5, 6 and 12 months after the medical record was opened (time 0). Due to the exiguous sample size, success rate was assessed only as intention-to-treat. Retention rate and attrition rate were estimated as the proportion of subjects still attending the treatment protocol at 1, 2, 3, 4, 5, 6 and 12 months of follow up.
All the dropouts after time 0 were recalled, in order to evaluate their smoking status.
Main predictors for smoking cessation were assessed by binary logistic regression.
Statistical analysis was carried out using IBM SPSS statistics version 25. A p-value of 0.05 was identified as threshold for statistical significance.
Results
Sample characteristics
Between February 2014 and December 2018, an overall number of 158 subjects were enrolled. Nearly 61% of them (n=97) joined the program and accessed to the first medical examination. They were both male and female, with a gender ratio of 1, with an average age of 54 (SD ± 10,49). Most of the enrolled subjects had a medium to high educational level (60.8%), were married or cohabiting (76.8%), and were regularly employed (77.9%). They were slightly overweight, with a mean body mass index of 27 Kg/m2 (SD ± 5,27), and most of them referred a sedentary lifestyle (25.8% did not engage in any regular physical activity). Furthermore, they daily consumed 1 unit of alcoholic beverage (SD ± 1,16) and almost 4 cups of coffee (SD ± 1,53). At the first medical evaluation, the enrolled subjects showed several comorbidities: respiratory disease (23.1%), gastro-esophageal disorders (34.4%) or sterility/erectile dysfunctions (4%), mostly being under treatment for them (77.1% of the subjects referred to take drugs).
Assessment of tobacco smoking habits
Enrolled subjects had been smoking for 37.5 years (SD ± 11.42), since the age of 16.5 (SD ± 4.89), an average amount of 23.7 (SD ± 12.32) cigarettes a day. Most of them had at least one relative with smoking habits (98.3% of the sample). They reported a previous attempt to quit smoking (86.6% of the study population), meanly lasted 33.3 months (SD ± 54.49), more frequently without a specialist support and by nicotine replacement therapy or electronic cigarette.
At the baseline, study population showed a high level of nicotine dependence, as evidenced by the Fagerström Test average score (5.4 ± SD 2.27), but with low levels of expired CO (18.2 ppm ± SD 9.27) and carboxyhemoglobin (COHb) (3.7% ± SD 1.5).
First psychological examination highlighted a high motivation to quit smoking: subjects believed they had a 60% chance of becoming non-smokers (score 6.2 at the self-efficacy test) and a high motivation, due to gain health (score 8.9 at motivational test), physical efficiency (score 5.6), and freedom from addiction (score 5.3).
Expired CO and carboxyhemoglobin (COHb) showed a significant decrease already two months after the first medical record: average expired CO reduced from 18.2 ppm to 5.7 ppm (p= 0.000) and mean COHb halved, switching from 3.7% to 1.6%.
Cascade analysis
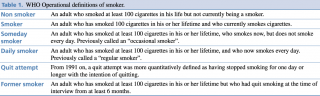
As shown in Figure 1, only 97 subjects (61.4% of those who participated to the first orientation meeting) accepted to continue with the first medical examination.
Cascade analysis Attrition Rate and Retention Rate
Eleven current smokers were still in the program at the time of the analysis and, therefore, excluded. Subjects who finally started the quit-smoking protocol (n=86; 54%) followed the program for an average time of 3.38 months (SD ± 3.71), with a significant difference (p= 0.000) between people who quitted smoking and people who didn’t. Those who had a negative outcome reported an average attendance of 1.9 months (SD ± 2.27), significantly (p= 0.000) different from those with a positive outcome, who had followed the intervention for 6.6 months (SD ± 4,18).
As shown in Figure 1, the retention rate decreased in three different moments: between the first orientation meeting and the opening of the medical records (54% of subjects started the course), at two months of treatment (56% of the subjects moved from the first month of treatment to the second), and between six months and one year. In this case 46% of the subjects attending the program at six months have also reached the twelve months of the program.
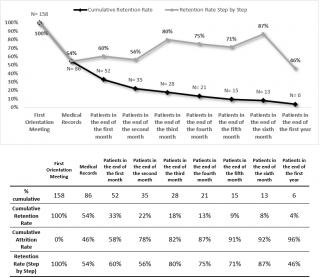
As illustrated in figure 2, 31.8% of subjects quitted smoking during the first month. The percentage of subjects who stopped smoking remained elevated till the end of the fourth month (24.2%), then progressively declined to 7.6% at the end of the protocol treatment (twelve months).
Percentage of smokers, former smokers and dropout in each stage of the program
One year after the beginning of treatment, 90.9% (n=60) of the study population dropped the program. Among these subjects, reached by telephone recall, 28.3% (n=17) had ceased smoking.
Univariate and Multivariate analysis
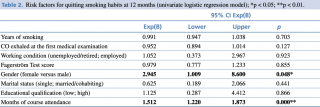
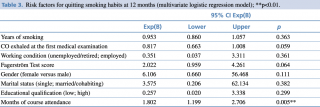
As shown in Tables 2 and 3, cigarette smoke abstinence at one year was significantly associated with the number of months of program attendance. For each additional month of program attendance there was an increased chance to quit smoking (OR 1.512; 95%CI 1.220-1.873, p 0.000), which was still significant at the multivariate logistic regression (OR 1.802; 95%CI 1.199-2.706, p 0.005). This probability was higher in men: women were less likely to reach the former-smoker status at 12 months (OR 2.945, 95% CI 1.009-8.600, p <0.05), although this result was not confirmed at multivariate analysis.
Table 2. Risk factors for quitting smoking habits at 12 months (univariate logistic regression model).
Table 3. Risk factors for quitting smoking habits at 12 months (multivariate logistic regression model).
Discussion
To the best of our knowledge, this is one of the few studies investigating the effectiveness of anti-smoking centers in Italy and the only one evaluating retention rate and attrition rate of the subjects’ joining a free territorial service dedicated to smoking cessation in Italy.
During the five years the quit-smoking program set out, an overall success rate of 18.2% was reached at 6 months, declining at one year. Indeed, only 7.6% of subjects joining the program reached the goal of 12 months of treatment. Success rate at one year was lower when compared to other experience,32,33,34 ranging from 27% to 39% at 12 months. The whole therapeutic process showed three critical moments, in which the retention rate sharply fell: from the first orientation meeting to the first medical examination, the transition between the first and the second month of treatment and from the sixth to the twelfth month.
Among the 158 subjects taking part to the first orientation meeting, only 61.4% (N=97) decided to join the program. This high dropout rate could be explained by the fact that subjects at their first access to CeSTab were in a “precontemplative” phase,29 generally driven by family or friends and not by personal motivation.
The transition to the second month of treatment and from the sixth to the twelfth month represents the second and the third weak point of the therapeutical chain. Albeit the explanations are quite controversial according to the Authors, a reason for the decrease in retention rate at these stages could be mainly found in organizational critical issues, such as short opening time of CeSTab during the week and lack of personnel.
The duration of course attendance is a main predictor of smoking cessation, as confirmed by univariate and multivariate analysis. After the adjustment for main confounding factors (gender, education, working condition, marital status, years of smoking, Fagerström test score, and exhaled carbon monoxide), each further month of compliance to the program significantly increased by more than 80% the probability to reach the goal of quitting smoking.
Results are in line with other studies showing that the duration of the therapeutic program was one of the most impacting predictive factors,32,36,38 especially when undertaken together with friends or family members.34 Conversely, some factors that showed a significant association in other works (such as nicotine addiction test, age of onset, previous attempts to quit smoking and so on),32,33,35-38 didn’t give similar results in our experience. However, it must be pointed out that the limited sample size of our work could affect the achievement of the significance threshold.
Strengths and limits
The present work represents a preliminary investigation, with some epidemiological limitations: the small sample size, the high number of dropouts, the incomplete medical records, the self-reference of the abstinence from tobacco evaluated only at the end of the program and not confirmed by biochemical verification, can expose the study to a risk of bias.
Conclusion and future perspectives
Local preventive interventions for smoking cessation, in particular those combining pharmacological and psychological therapy, increases the probability of successfully quitting smoking. The longer the subjects attend the course, the higher is the change to become former smokers.
However, a significant attention should be paid on the first stages of the program, that are undoubtedly the weakest point of the process, in order to increase retention rate and, therefore, improve success chances. This goal can be achieved by improving the service management: for instance, wider opening hours per week and enhancing human resources engaged in the service, are recommended, in order to implement the therapeutic strategy.
In addition, extending access to the quit smoking service to a larger population could be useful: since the prevalence of smokers in Italy is nearly 25% among men and 20% among women,3 in the area covered by the Local Health Unit nearly 100.000 smokers can be estimated. Among them, between 30% and 50% want to quit smoking, according to the international studies.39-40 Therefore, CeSTab activities should be improved, in order to cover a much higher and significant part of the potential users. An active strategy of case finding aimed at informing and recruiting the target population is a priority for an effective intervention of the anti-smoking center. Workplaces or areas of social aggregation could then become the successful setting of future enrollment programs, particularly focused on the young people and workers.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Acknowledgments
None.
References
- Peacock A., Leung J., Larney S., Colledge S., Hickman M., Rehm J., Giovino G.A., West R., Hall W., Griffiths P., Ali R., Gowing L., Marsden J., Ferrari A.J., Grebely J., Farrell M., Degenhardt L. Global Statistics on Alcohol, Tobacco and Illicit Drug Use: 2017 Status Report. Addiction. 2018 Oct;113(10):1905-1926. doi: 10.1111/add.14234. Epub 2018 Jun 4.
- WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies ISBN 978-92-4-151282-4
- L’abitudine al fumo in Italia, Dati 2014-2017 del sistema di sorveglianza PASSI.
- Balfour D.J., Wright A.E., Benwell M.E., Birrell C.E. The Putative Role of Extra-Synaptic Mesolimbic Dopamine in the Neurobiology of Nicotine Dependence. Behav Brain Res 2000; 113:73-83
- Dani J.A., Heinemann S. Molecular and Cellular Aspects of Nicotine Abuse. Neuron 1996; 16:905-908
- Dani J.A., De Biasi M. Cellular Mechanisms of Nicotine Addiction. Pharmacol Biochem Behav 2001; 70:439-446
- Di Chiara G. Role of Dopamine in the Behavioural Actions of Nicotine Related to Addiction. Eur J Pharmacol 2000; 393:295-314.
- Schelling T.C. Addictive Drugs: The Cigarette Experience. Science 1992; 255:430-433
- Stolerman I.P., Shoaib M. The Neurobiology of Tobacco Addiction. Trends Pharmacol Sci 1991; 12:467-473
- Broide R.S., Leslie F.M. The Alpha7 Nicotinic Acetylcholine Receptor in Neuronal Plasticity. Mol Neurobiol 1999; 20:1-16
- Dani J.A. Overview of Nicotinic Receptors and Their Roles in the Central Nervous System. Biol Psychiatry 2001; 49:166-174.
- Guo J.Z., Tredway T.L., Chiappinelli V.A. Glutamate and GABA Release Are Enhanced by Different Subtypes of Presynaptic Nicotinic Receptors in the Lateral Geniculate Nucleus. J Neurosci 1998; 18:1963-1969.
- Li X., Rainnie D.G., McCarley R.W., Greene R.E. Presynaptic Nicotinic Receptors Facilitate Monoaminergic Transmission. Journal of Neuroscience 1998; 18:1904-1912.
- Radcliffe K.A, Dani J.A. Nicotinic Stimulation Produces Multiple Forms of Increased Glutamatergic Synaptic Transmission. J Neurosci 1988; 18:7075-7083
- Mansvelder H.D., McGehee D.S. Long-Term Potentiation of Excitatory Inputs to Brain Reward Areas by Nicotine. Neuron 2000; 27:349-357
- Benowitz N.L., Porchet H., Jacob P. Nicotine Dependence and Tolerance in Man: Pharmacokinetic and Pharmacodynamic Investigations. Prog Brain Res 1989; 79:279-287
- Russell M.A. Subjective and Behavioural Effects of Nicotine in Humans: Some Sources of Individual Variation. Prog Brain Res 1989; 79:289-302.
- Buisson B., Bertrand D. Chronic Exposure to Nicotine Upregulates the Human (Alpha)4((Beta)2 Nicotinic Acetylcholine Receptor Function. J Neurosci 2001; 21:1819-1829
- Trauth J.A., Seidler F.J., McCook E.C., Slotkin T.A. Adolescent Nicotine Exposure Causes Persistent Upregulation of Nicotinic Cholinergic Receptors in Rat Brain Regions. Brain Res 1999; 851:9-19
- Pauly J.R., Marks M.J., Robinson S.F., van de Kamp J.L., Collins AC. Chronic Nicotine and Mecamylamine Treatment Increase Brain Nicotinic Receptor Binding without Changing Alpha 4 Or Beta 2 Mrna Levels. J Pharmacol Exp Ther 1996; 278:361-369
- Balfour D.J., Fagerstrom K.O. Pharmacology of Nicotine and Its Therapeutic Use in Smoking Cessation and Neurodegenerative Disorders. Pharmacol Ther 1996; 72:51-81
- Dani J.A., Ji D., Zhou F.M. Synaptic Plasticity and Nicotine Addiction. Neuron 2001; 31:349-352
- Whittaker R., Borland R., Bullen C., Lin R.B., McRobbie H., Rodgers A. Mobile Phone-Based Interventions for Smoking Cessation. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No.: CD006611. DOI: 10.1002/14651858.CD006611.pub2
- Park E.W., Schultz J.K., Tudiver F.G., Campbell T., Becker L.A. Enhancing Partner Support to Improve Smoking Cessation. Cochrane Database of Systematic Reviews 2004, Issue 3. Art. No.: CD002928. DOI: 10.1002/14651858.CD002928.pub2
- Civljak M., Sheikh A., Stead L.F., Car J. Internet-Based Interventions for Smoking Cessation. Cochrane Database of Systematic Reviews 2010, Issue 9. Art. No.: CD007078. DOI: 10.1002/14651858.CD007078.pub3
- Stead L.F., Bergson G., Lancaster T. Physician Advice for Smoking Cessation. Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No.: CD000165. DOI: 10.1002/14651858.CD000165.pub3
- Cahill K., Perera R. Quit and Win Contests for Smoking Cessation. Cochrane Database of Systematic Reviews 2008, Issue 4.Art. No.: CD004986. DOI: 10.1002/14651858.CD004986.pub3
- Linee guida per il trattamento della dipendenza da tabacco, European Network for Smoking and Tobacco Prevention ENSP, SITAB, 2018
- Prochaska J.O., DiClemente C.C. Transtheoretical therapy: Toward A More Integrative Model of Change. Psychother. Theory Res. Pract. 1982, 19, 276
- Heatherton T.F., Kozlowski L.T., Frecker R.C., Fagerström K.O. The Fagerström Test for Nicotine Dependence: A Revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991 Sep;86(9):1119-27
- Global Adult Tobacco Survey Collaborative Group. Tobacco Questions for Surveys: A Subset of Key Questions from the Global Adult Tobacco Survey (GATS), 2nd Edition. Atlanta, GA: Centers for Disease Control and Prevention, 2011
- Marino M.G., Fusconi E., Magnatta R., Panà A., Maurici M. Epidemiologic Determinants Affecting Cigarette Smoking Cessation: A Retrospective Study in a National Health System (SSN) Treatment Service in Rome (Italy). J Environ Public Health. 2010;2010:183206. doi: 10.1155/2010/183206. Epub 2010 Apr 13.
- Belleudi V., Bargagli A.M., Davoli M., Di Pucchio A., Pacifici R., Pizzi E., Zuccaro P., Perucci C.A. Gruppo di Studio dei Servizi Territoriali per la Cessazione dal Fumo. [Characteristics and Effectiveness of Smoking Cessation Programs in Italy. Results of a Multicentric Longitudinal Study]. Epidemiol Prev. 2007Mar-Jun;31(2-3):148-57. Italian. PubMed PMID: 18677864.
- Picardi A., Bertoldi S., Morosini P. Association Between the Engagement of Relatives in a Behavioural Group Intervention for Smoking Cessation and Higher Quit Rates at 6-, 12- And 24-Month Follow-Ups. Eur Addict Res. 2002 Jun;8(3):109-17.
- Caponnetto P., Polosa R. Common Predictors of Smoking Cessation in Clinical Practice. Respir Med. 2008 Aug;102(8):1182-92. doi: 10.1016/j.rmed.2008.02.017. Epub 2008 Jun 30.
- Iliceto P., Fino E., Pasquariello S., D'Angelo Di Paola M.E., Enea D. Predictors of Success in Smoking Cessation among Italian Adults Motivated to Quit. J Subst Abuse Treat. 2013 May-Jun;44(5):534-40. doi: 10.1016/j.jsat.2012.12.004. Epub 2013 Jan 9.
- Gorini G., Chellini E., Terrone R., Ciraolo F., Di Renzo L., Comodo N. Course on Smoking Cessation Organized by the Italian League Against Cancer in Florence: Determinants of Cessation at the End of the Course and After 1 Year. Epidemiologia e Prevenzione, vol. 22, no. 3, pp. 165–170, 1998.
- Gorini G., Morasso G., Alberisio A. Smoking Cessation Course Organized by the Italian League for the Fight against Tumors in Milan and Rome: Determinants of Cessation after the Course and after A Year. Epidemiologia e Prevenzione, vol. 25, no. 3, pp. 113–117, 2001.
- Mathur S., Singh N. Characteristics of Smokers with Intentions to Quit, with a Focus on Occupational Status, Race/Ethnicity, and Cognitive Behaviour. Epidemiology Biostatistics and Public Health - 2015, Volume 12, Number 1
- Abdullah AS, Yam HK. Intention to Quit Smoking, Attempts to Quit, and Successful Quitting among Hong Kong Chinese Smokers: Population Prevalence and Predictors. Am J Health Promot. 2005 May-Jun;19(5):346-54.